Top Recommendations for the Diagnosis and Management of Esophagogastric Variceal Bleeding
Prateek Sharma, MD, FASGE, reviewing Gralnek IM, et al. Endoscopy 2022 Sep 29.
The European Society of Gastrointestinal Endoscopy has released updated recommendations on the diagnosis and management of esophagogastric variceal hemorrhage. Of the 16 recommendations, all are considered “strong” recommendations, and the quality of evidence is indicated as high for 8 recommendations, moderate for 7, and low for one. Here are the top recommendations:
- If there are no contraindications, patients with compensated advanced chronic liver disease (ACLD; due to viruses, alcohol, and/or nonobese [body mass index <30kg/m2] nonalcoholic steatohepatitis) and clinically significant portal hypertension (hepatic venous pressure gradient >10mmHg and/or liver stiffness by transient elastography >25 kPa) should be given nonselective beta-blocker (NSBB) therapy (preferably carvedilol) to prevent variceal bleeding. (Strong recommendation, moderate-quality evidence)
- Endoscopic band ligation (EBL) is the preferred endoscopic prophylactic treatment in patients unable to receive NSBB therapy for high-risk esophageal varices demonstrated by upper GI endoscopy screening. EBL should be repeated every 2 to 4 weeks until variceal eradication is achieved, followed by surveillance EGD performed every 3 to 6 months the first year after eradication. (Strong recommendation, moderate-quality evidence)
- Treatment with a vasoactive agent (terlipressin, octreotide, or somatostatin) should be initiated at the time of presentation in patients with suspected acute variceal bleeding and continued for up to 5 days. (Strong recommendation, high-quality evidence)
- Patients with ACLD presenting with acute esophageal variceal hemorrhage (EVH) should receive 1g daily of the antibiotic prophylaxis ceftriaxone for up to 7 days. Alternative antibiotics may also be used based on local antibiotic resistance and patient allergies. (Strong recommendation, high-quality evidence)
- Provided there are no contraindications, patients with suspected acute EVH should be given 250 mg of intravenous erythromycin 30 to 120 minutes before upper GI endoscopy. (Strong recommendation, high-quality evidence)
- Patients with suspected EVH should undergo endoscopic evaluation within 12 hours of presentation, as long as hemodynamic resuscitation has been performed. (Strong recommendation, moderate-quality evidence)
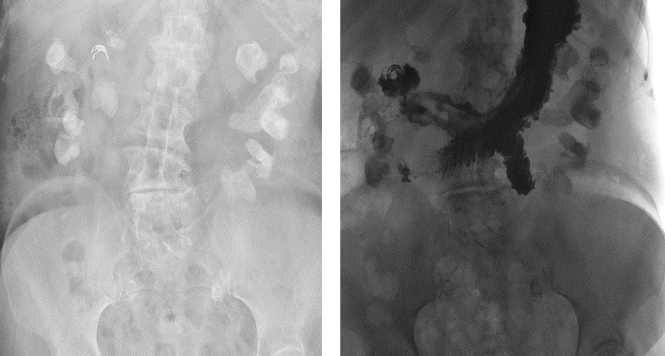
- An endoscopic cyanoacrylate injection for acute gastric (cardiofundal) variceal (GOV2, IGV1) hemorrhage should be administered. (Strong recommendation, moderate-quality evidence)
- Patients who have undergone EBL for acute EVH should receive follow-up EBLs every 1 to 4 weeks until esophageal varices are eradicated (secondary prophylaxis). (Strong recommendation, moderate-quality evidence)

COMMENTEarly endoscopy in patients with suspected variceal bleeding, use of antibiotics in those with cirrhosis, and consideration of beta blockers for primary prevention are all important strategies to improve patient outcomes.
Note to readers: At the time we reviewed this paper, its publisher noted that it was not in final form and that subsequent changes might be made.
CITATION(S)
Gralnek IM, Camus Duboc M, Garcia-Pagan JC, et al Endoscopic diagnosis and management of esophagogastric variceal hemorrhage: European Society of Gastrointestinal Endoscopy (ESGE) Guideline. Endoscopy 2022 Sep 29. (Epub ahead of print) (https://doi.org/10.1055/a-1939-4887)