European Society of Gastrointestinal Endoscopy Issues Guideline on Lower GI Tract Endoscopic Tissue Sampling
Douglas K. Rex, MD, MASGE, reviewing Pouw RE, et al. Endoscopy 2021 Oct 29.
These evidence-based recommendations from the European Society of Gastrointestinal Endoscopy (ESGE) cover principles of tissue sampling and removal in the lower GI tract. Some points from the guideline that likely differ from practice include:
- If colitis is suspected by endoscopy, perform segmental biopsies (at least 2 from each segment) of the ileum, cecum, ascending, transverse, descending, and sigmoid colon, and rectum, with samples from each area placed into separate bottles. This approach enables almost complete accuracy in differentiating among inflammatory bowel disease (IBD), infections, graft-vs-host disease, microscopic colitis, nonsteroidal anti-inflammatory drug-induced colitis, and amyloidosis.
- For suspected microscopic colitis, put 2 biopsy samples from the left hemicolon (descending and sigmoid) in 1 bottle and 2 from the right (ascending and transverse) in a separate bottle.
- For surveillance in IBD, use real or virtual chromoendoscopy with targeted biopsies. For high-risk patients, consider combining chromoendoscopy with 4-quadrant nontargeted biopsies every 10 cm.
- For pouch surveillance for dysplasia, target biopsies to suspicious endoscopic abnormalities and also take 2 tissue samples each from the afferent ileal loop, efferent blind loop, pouch, and anorectal cuff and place them in 4 separate bottles.
- Do not take biopsy samples from patients with Crohn’s disease to assess disease activity.
- To assess ulcerative colitis disease activity or remission, take at least 2 biopsy specimens from the worst affected area to examine for cytomegalovirus activity or presence. In endoscopically quiescent disease, consider biopsies to establish histologic remission.
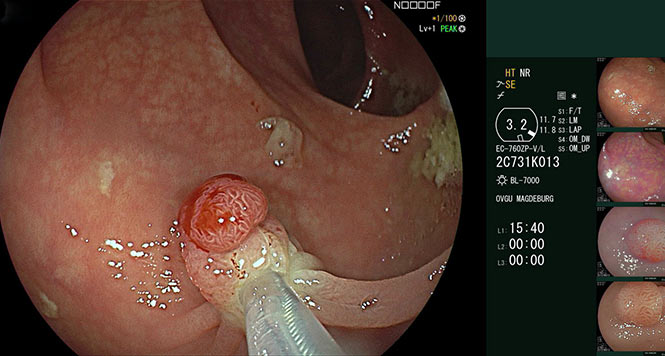
- Potentially malignant colorectal polyps should be excised en bloc rather than evaluated with a biopsy.
- If an endoscopist cannot confidently perform an en bloc excision, take representative images (not biopsy samples) from the worrisome area and refer the patient to an expert center.
- If endoscopic features of deep submucosal invasion indicate endoscopic excision is inappropriate, take 6 targeted biopsy samples from the potential cancer focus.
- Perform biopsies of cancers last (after all polypectomy, other biopsies, and tattooing) to avoid tumor seeding.

COMMENTNearly all of these recommendations were ranked as strong with low quality of evidence. The ESGE does a nice job of making recommendations that are clear and practical for endoscopists. One of the downsides of the guideline is the frequent recommendation to send multiple bottles to pathology. In some situations with low-quality evidence, this will lead to increased costs. Further, there is hardly agreement across or within countries and continents about which endoscopic features and their association with cancer risk warrant en bloc excision. This disagreement is the real challenge in recommending en bloc excision.
Note to readers: At the time we reviewed this paper, its publisher noted that it was not in final form and that subsequent changes might be made.
CITATION(S)
Pouw RE, Bisschops R, Gecse KB, et al. Endoscopic tissue sampling – part 2: lower gastrointestinal tract. European Society of Gastrointestinal Endoscopy (ESGE) guideline. Endoscopy 2021 Oct 29. (Epub ahead of print) (https://doi.org/10.1055/a-1671-6336)