Impact of Preresection Biopsy on Subsequent Endoscopic Mucosal Resection
Douglas K. Rex, MD, MASGE, reviewing Ma MX, et al. Endoscopy 2022 Jul 11.
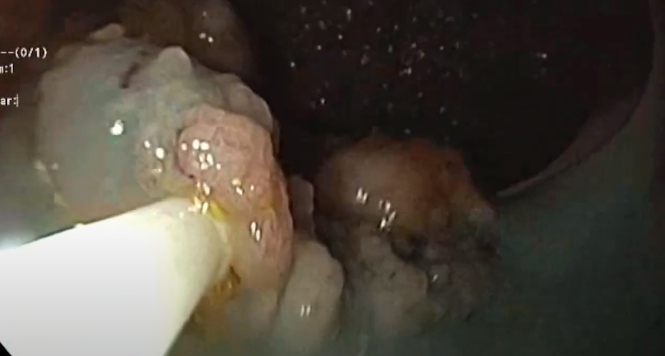
We often hear that physician-identified large nonpedunculated colorectal polyps (LNPCPs) that warrant referral to an advanced endoscopist for endoscopic mucosal resection (EMR) or endoscopic submucosal dissection should not undergo preresection biopsy because it increases submucosal fibrosis. This recommendation is largely based on anecdotal evidence.
In this study of 586 LNPCPs, lesions that had undergone biopsy before EMR were larger than those without preresection biopsy (median, 35 mm vs 30 mm). The histology from the preresection biopsy was upstaged in 26% of LNPCP specimens, downstaged in 14%, and unchanged in 60% after EMR. Sensitivity of preresection biopsy for high-grade dysplasia was only 21%. None of the 19 lesions with cancer were predicted by preresection biopsy.
Preresection biopsy was associated with a higher rate of intraprocedural bleeding during EMR (31.5% vs 23.5%; P=.033) but was not associated with delayed bleeding or perforation, or even deep mural injury. Success of EMR and endoscopic recurrence rates were not affected by preresection biopsy.
Submucosal fibrosis was found more often in lesions with preresection biopsy (43.1% vs 30%; P=.001).

COMMENTThe poor sensitivity of preresection biopsy for cancer probably reflects referral bias because preresection biopsies that diagnosed cancer would lead to surgical referral rather than endoscopic resection. Having said that, the only rational reason to perform preresection biopsy is to identify cancer, and the real question is how often cancer is identified by a preresection biopsy when there is no overt endoscopic evidence of cancer. This study can’t answer that question, but the likely answer is “almost never.”
This study does suggest that preresection biopsy of benign-appearing laterally spreading lesions produces some problems for EMR, including submucosal fibrosis and increased intraprocedural bleeding. Overall, the study supports the recommendation to not perform a biopsy of laterally spreading lesions unless there is overt evidence of cancer. It indirectly supports the common admonition to avoid performing biopsies of flat areas and the edges of lesions, which are more likely to lead to significant submucosal fibrosis. This could alter the subsequent resection approach compared to biopsy of bulky or sessile portions of the lesion.
Note to readers: At the time we reviewed this paper, its publisher noted that it was not in final form and that subsequent changes might be made.
CITATION(S)
Ma MX, Tate DJ, Sidhu M, Zahid S, Bourke MJ. Pre-resection biopsy of large non-pedunculated colorectal polyps does not reliably detect advanced dysplastic change and may increase complexity of endoscopic mucosal resection. Endoscopy 2022 Jul 11. (Epub ahead of print) (https://doi.org/10.1055/a-1896-9798)