New Expert Review From the American Gastroenterological Association on Managing Colonic Diverticulitis
Douglas K. Rex, MD, MASGE, reviewing Peery AF, et al. Gastroenterology 2020 Dec 3.
The American Gastroenterological Association has issued a clinical practice update on the management of colonic diverticulitis. The recommendations are as follows:
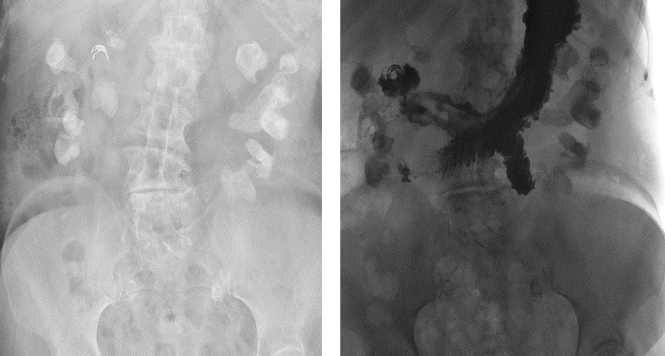
- Physicians should order a CT at least once to confirm that symptoms are related to diverticulitis. CT should also be used to evaluate potential complications, severe presentations, failure to improve on treatment, immunocompromised patients, and patients with multiple recurrences who are contemplating surgery.
- Colonoscopy is advised after complicated diverticulitis and after an initial episode of uncomplicated diverticulitis unless there has been a high-quality colonoscopy in the past year.
- Colonoscopy should be delayed 6 to 8 weeks after an acute episode or until symptom resolution, whichever is longer. Colonoscopy can be performed earlier if there are alarm symptoms.
- In patients with persistent symptoms, both a CT and colonoscopy should be performed. If the workup is negative, gastroenterologists should consider visceral hypersensitivity.
- Patients should be advised to use clear liquids during an acute attack and advance as tolerated.
- Immunocompetent patients with mild, uncomplicated diverticulitis can be treated selectively with antibiotics.
- Antibiotics are advised for frail patients and patients who have uncomplicated diverticulitis with comorbidities, refractory symptoms or vomiting, a C-reactive protein level >140 mg/L, or a white blood cell count >15.
- Antibiotics are warranted for complicated diverticulitis or if a fluid collection or long segment of inflammation is detected on a CT.
- Immunocompromised patients warrant a low threshold for antibiotics, CT, and surgical consultation.
- To reduce recurrence, patients should be advised to observe a high-quality diet, normal weight, physical activity, smoking cessation, and nonsteroidal anti-inflammatory drug avoidance (except medically indicated aspirin therapy). Probiotics, 5-aminosalicylates, and rifaximin are ineffective.
- The first episode is usually the worst. In patients with recurrent uncomplicated episodes, surgery should not be advised. The decision should be individualized. Surgery may not eliminate chronic symptoms.

COMMENTThe risk of perforation from colonoscopy in the period after an acute episode is mostly theoretical. I have performed colonoscopy within a 4-week window many times and have not seen a complication. If symptoms, such as concurrent rectal bleeding or iron deficiency anemia, warrant colonoscopy, it’s reasonable to proceed. Water filling during insertion, rather than gas insufflation, is prudent.
Note to readers: At the time we reviewed this paper, its publisher noted that it was not in final form and that subsequent changes might be made.
CITATION(S)
Peery AF, Shaukat A, Strate LL. AGA clinical practice update on medical management of colonic diverticulitis: expert review. Gastroenterology 2020 Dec 3. (Epub ahead of print) (https://doi.org/10.1053/j.gastro.2020.09.059)