ESD probably no better than EMR in Barrett’s neoplasia
Thomas Rösch, Hamburg
Gut. 2016 Jan 22. pii: gutjnl-2015-310126. [Epub ahead of print]
| A randomised trial of endoscopic submucosal dissection versus endoscopic mucosal resection for early Barretts`s neoplasia |
| Grischa Terheggen1, Eva Maria Horn2, Michael Vieth3, Helmut Gabbert4, Markus Enderle5, Alexander Neugebauer5, Brigitte Schumacher6, Horst Neuhaus2 |
Background
For endoscopic resection of early GI neoplasia, endoscopic submucosal dissection (ESD) achieves higher rates of complete resection (R0) than endoscopic mucosal resection (EMR). However, ESD is technically more difficult and evidence from randomized trial is missing.
Objective
We compared the efficacy and safety of ESD and EMR in patients with neoplastic Barrett’s oesophagus (BO). Design BO patients with a focal lesion of high-grade intraepithelial neoplasia (HGIN) or early adenocarcinoma (EAC) ≤3 cm were randomized to either ESD or EMR. Primary outcome was R0 resection; secondary outcomes were complete remission from neoplasia, recurrences and adverse events (AEs).
Results
There were no significant differences in patient and lesion characteristics between the groups randomised to ESD (n=20) or EMR (n=20). Histology of the resected specimen showed HGIN or EAC in all but six cases. Although R0 resection defined as margins free of HGIN/EAC was achieved more frequently with ESD (10/17 vs 2/17, p=0.01), there was no difference in complete remission from neoplasia at 3 months (ESD 15/16 vs EMR 16/17, p=1.0). During a mean follow-up period of 23.1±6.4 months, recurrent EAC was observed in one case in the ESD group. Elective surgery was performed in four and three cases after ESD and EMR, respectively (p=1.0). Two severe AEs were recorded for ESD and none for EMR ( p=0.49).
Conclusions
In terms of need for surgery, neoplasia remission and recurrence, ESD and EMR are both highly effective for endoscopic resection of early BO neoplasia. ESD achieves a higher R0 resection rate, but for most BO patients this bears little clinical relevance. ESD is, however, more time consuming and may cause severe AE.
What you need to know
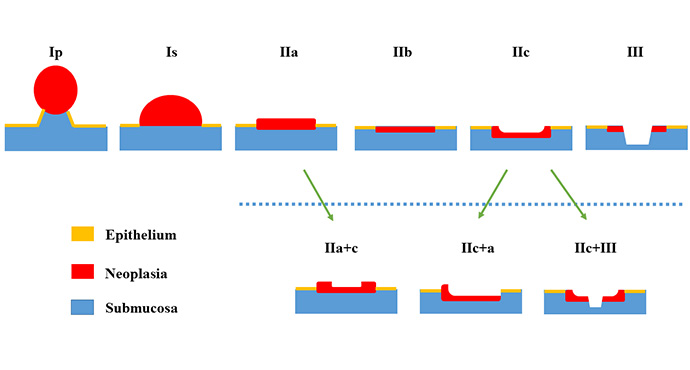
Considerable debate is currently taking place among therapeutic endoscopists regarding the best method of resecting early carcinomas, particularly in the upper gastrointestinal tract — whereas the corresponding debate regarding the colorectum is somewhat more difficult, due to the biological differences. The methods that were compared here were endoscopic mucosal resection (EMR) and endoscopic submucosal dissection (ESD). In the latter procedure, an effort is made to resect the lesion en bloc, while EMR has to make do with piecemeal ablation of the tumor, particularly with lesions larger than 2 cm.
In general, the discussion is not based on high-grade evidence, as there has not been a single no randomized study on EMR versus ESD, even though in Japan and other East Asian countries thousands of procedures are carried out every year. The impression is given by so-called meta-analyses of retrospective studies that ESD is superior to EMR with regard to the rates of complete R0 resection and the recurrence rate, although it is associated with a significantly larger number of complications. “Meta-analyses” of this type have been carried out for EMR versus ESD and for ESD alone with squamous cell carcinoma of the esophagus [1], gastric carcinoma [2–4], and colorectal neoplasia [5,6].
This study by the Düsseldorf group, the first randomized study on ESD versus EMR, is therefore very welcome, although it is a small one and only surrogate parameters were used for the outcome. Forty patients with visible focal Barrett’s neoplasia with high-grade dysplasia or early carcinoma were randomly assigned to undergo focal resection of the lesion either with EMR or ESD. Subsequently, the residual Barrett’s segment was eradicated using radiofrequency ablation. The primary outcome was R0 resection, and the large differences that were expected here permitted the relatively small number of patients in the sample size calculation. The study was therefore not sufficiently powered for the secondary outcome — i.e., complete remission of neoplasia and/or Barrett’s esophagus — as the number of cases was too small. Endoscopic follow-up examinations were carried out after 3, 6, 9, and 12 months; the mean follow-up period was 23 months in both groups.
Not unexpectedly, the results show that ESD is superior with regard to complete and R0 resection, although the findings were less spectacular than expected. However, the follow-up results did not differ with regard to the outcome , with only one local recurrence developing — which was in the ESD group. Details are shown in the following table. Three patients were excluded from each group, as the histological findings showed a normal Barrett’s segment or only low-grade dysplasia despite initial biopsy diagnoses in accordance with the inclusion criteria (see above).
| Parameter | ESD | EMR | p |
|---|---|---|---|
| N | 20 | 20 | |
| Histology | |||
| HGIN | 0 | 2 | |
| T1 m | 10 | 12 | |
| T1 sm1 | 6 | 2 | |
| Complete R0 resection | 10/17 | 2/17 | 0.01 |
| Curative resection* | 15/17 | 4/17 | |
| Procedure duration | 54 min | 22 min | 0.00002 |
| Severe AE** | 2* | 0 | |
| 30-day mortality | 0 | 0 | |
| Follow-up | |||
| Complete remission | 16/16 | 17/17 | |
| Recurrence | 1 | 0 |
* Patients with infiltration deeper than the mucosa were not counted as curative. * One case of mediastinitis. AE=adverse event
As the table shows, two perforations occurred in the ESD group, one of which led to mediastinitis, while no severe complications were noted in the EMR group. Similarly, after complete remission with both resection procedures in combination with ablation in all cases, the only local recurrence was found in the ESD group. For both types of event (complications / recurrence rate), however, the case numbers were too small for statistically valid conclusions to be drawn. The authors attempt to use these data as the basis for a sample size calculation for a randomized outcome study and conclude that a study of that type would require more than 500 patients, in view of the very high ultimate remission rates with Barrett’s and Barrett’s neoplasia in combination with resection and ablation. It is debatable whether extrapolations of that type are admissible on the basis of a small pilot study. Overall, of course, there are very good data on the long-term success of EMR [7,8] and also good data on ESD [9–11] in Barrett’s esophagus with neoplasia, although usually with one of the other forms of thermoablation.
Although only surrogate parameters (R0 resection) were used in this study, two aspects of it are interesting beyond the immediate results. With regard to the question of whether R0 resection is relevant, the answer is formally no with most EMRs (due to piecemeal resection). In view of the high rate of complete eradication of Barrett’s/Barrett’s neoplasia, which seems to be quite similar to that with ESD (in combination with thermoablation methods, of course), the question may be permitted of whether early carcinomas could be oncologically safely resected as well. In addition, the recurrence rate for EMR within 2 years does not appear to be massively higher than that with ESD. However, both of these conclusions must be treated with caution, as the case numbers were not large enough for statistical validity. It should also be borne in mind that neoplastic Barrett’s esophagus represents a special case in comparison with other types of early carcinoma in the upper gastrointestinal tract: several stages of neoplasia may occur simultaneously or one after another in various locations in the same Barrett’s segment. The ultimate goal is therefore complete eradication of the neoplastic Barrett’s esophagus and not only focal resection of the (recognizable) neoplasia present in it. It can be concluded from this preliminary study that this goal can be achieved with similar or not substantially different rates of success using both resection procedures in combination with thermoablation, and this should be taken into account in the definition of primary outcomes in further large-scale randomized studies.
References
- Kim JS, Kim BW, Shin IS. Efficacy and safety of endoscopic submucosal dissection for superficial squamous esophageal neoplasia: a meta-analysis. Dig Dis Sci 2014;59:1862-9.
- Cao Y, Liao C, Tan A, et al. Meta-analysis of endoscopic submucosal dissection versus endoscopic mucosal resection for tumors of the gastrointestinal tract. Endoscopy 2009;41:751-7.
- Facciorusso A, Antonino M, Di Maso M, et al. Endoscopic submucosal dissection vs endoscopic mucosal resection for early gastric cancer: A meta-analysis. World J Gastrointest Endosc 2014;6:555-63.
- Park YM, Cho E, Kang HY, et al. The effectiveness and safety of endoscopic submucosal dissection compared with endoscopic mucosal resection for early gastric cancer: a systematic review and metaanalysis. Surg Endosc 2011;25:2666-77.
- Fujiya M, Tanaka K, Dokoshi T, et al. Efficacy and adverse events of EMR and endoscopic submucosal dissection for the treatment of colon neoplasms: a meta-analysis of studies comparing EMR and endoscopic submucosal dissection. Gastrointest Endosc 2015;81:583-95.
- Wang J, Zhang XH, Ge J, et al. Endoscopic submucosal dissection vs endoscopic mucosal resection for colorectal tumors: a meta-analysis. World J Gastroenterol 2014;20:8282-7.
- Pech O, Bollschweiler E, Manner H, et al. Comparison between endoscopic and surgical resection of mucosal esophageal adenocarcinoma in Barrett‘s esophagus at two high-volume centers. Ann Surg 2011;254:67-72.
- Pech O, May A, Manner H, et al. Long-term efficacy and safety of endoscopic resection for patients with mucosal adenocarcinoma of the esophagus. Gastroenterology 2014;146:652-660.e1.
- Chevaux JB, Piessevaux H, Jouret-Mourin A, et al. Clinical outcome in patients treated with endoscopic submucosal dissection for superficial Barrett‘s neoplasia. Endoscopy 2015;47:103-12.
- Hobel S, Dautel P, Baumbach R, et al. Single center experience of endoscopic submucosal dissection (ESD) in early Barrett‘s adenocarcinoma. Surg Endosc 2015;29:1591-7.
- Park CH, Kim EH, Kim HY, et al. Clinical outcomes of endoscopic submucosal dissection for early stage esophagogastric junction cancer: a systematic review and meta-analysis. Dig Liver Dis 2015;47:37-44.