Esophageal duplication cysts (EDCs)
Kozłowska-Petriczko K (1), Pawlak K (2), Wiechowska-Kozłowska A (2)
1.SPWSZ Arkonska Hospital, Szczecin, Poland | 2. Hospital of the Ministry of Interior and Administration, Department of Internal Medicine, Cardiology, Gastroenterology and Endocrinology, Szczecin, Poland
Esophageal duplication cysts (EDCs) are rare, congenital anomalies with prevalence of about 0.0122%. EGD are located most commonly in the lower one third of the esophagus. As mainly asymptomatic lesions, they are usually an incidental finding in routine endoscopy. Based on their morphologic endoscopic features they can be classified as submucosal lesions. Duplication cysts can be visualized with many imaging modalities, from more basic such as a chest x-ray, to more advanced, e.g. mediastinal magnetic resonance imaging. However, the only examination which can differentiate duplication cysts with other submucosal pathologies is an endoscopic ultrasound with duplex Doppler imaging.
Here we present a case of a patient qualified for endosonographic evaluation of unspecific esophageal submucosal lesion (SEL). The lesion was detected during routine upper GI endoscopy performed before planned cholecystectomy. The patient was without symptoms.
EUS imaging showed hypoechogenic, anechoic cystic lesion with regular wall, with no blood flow in duplex Doppler examination. With such a typical image a biopsy was not required to confirm the diagnosis of single esophageal duplication cyst.
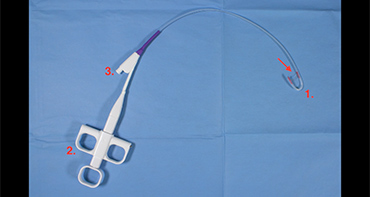
Figure 1. Left- EDC in EUS. EUS imaging showed hypoechogenic, anechoic cystic lesion with regular wall, with no blood flow in duplex Doppler examination. Right- Endoscopy od upper GIT. Submucosal lesions covered by normal mucosa, without typical symptoms for gastric varices. There is no possibility to differentiate SEL.
Endoscopic view
- Submucosal lesions covered by normal mucosa, without typical symptoms for gastric varices.
- EGD does not allow for differentiation of submucosal lesions and gastric varices.
Endoscopic ultrasound
- Periesophageal homogenous hypoechoic, anechoic cyst, with multi-layered wall, well-defined margins, can include fluid with debris.
- Doppler color evaluation- without blood flow.
- Allows differentiate esophageal lesions from bronchogenic lesions. Typical for EDCs are: proximity to the esophagus, absence of cartilage, and the presence of a double muscle layer covering the cyst.
- EUS is a useful tool for differentiating between cystic and solid esophageal lesions like esophageal leiomyoma. Moreover, use of color Doppler allows for differentiation between gastric varices and EDC
Diagnosis, furtherer follow-up, treatment
- Biopsy is not required in patients with typical endosonographic view. Moreover, biopsy is related with a 14% risk of infection. The exceptions are lesions with an unusual appearance and oncological potential.
- Follow-up is not necessary. Versleijen et al. presented follow-up of EDC over 13 years without progression, complication and malignant transformation. Malignancy is rare, but the exact rate is uncertain.
- Surgical treatment in the case of symptomatic illness or the presence of complications.
References
- Liu R, Adler DG. Duplication cysts: Diagnosis, management, and the role of endoscopic ultrasound. Endosc Ultrasound. 2014;3(3):152–160.
- Timothy A. Plerhoples MD, Thomas M. Krummel MD, in Kendig & Chernick’s Disorders of the Respiratory Tract in Children (Eighth Edition), 2012.
- Versleijen MW, Drenth JP, Nagengast FM. A case of esophageal duplication cyst with a 13-year follow-up period. Endoscopy. 2005;37:870–2.
- Al-Riyami S, Al-Sawafi Y. True Intramural Esophageal Duplication Cyst. Oman Med J. 2015;30(6):469–472.
Authors:
Kozłowska-Petriczko K (1), Pawlak K (2), Wiechowska-Kozłowska A (2)
1.SPWSZ Arkonska Hospital, Szczecin, Poland
2. Hospital of the Ministry of Interior and Administration, Department of Internal Medicine,
Cardiology, Gastroenterology and Endocrinology, Szczecin, Poland