Nonendoscopic Screening for Barrett’s Esophagus: Are We There?
Prateek Sharma, MD, FASGE, reviewing Iyer PG, et al. Am J Gastroenterol 2020 Jun 15.
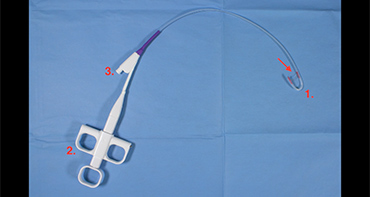
Upper endoscopy (EGD) with biopsy remains the gold standard for the diagnosis of Barrett’s esophagus (BE). Several nonendoscopic techniques (sponge, capsule) have utilized biomarkers, such as protein markers, microRNAs, and methylated DNA markers, as screening tools for BE. This multicenter case-control study was designed to evaluate the accuracy of a sponge-on-string device (EsophaCap, Capnostics, Pa) for BE diagnosis.
A total of 112 BE cases (≥1 cm of circumferential BE with intestinal metaplasia; median age, 66 years; 82% male; median BE segment length, C4M6; 49% no dysplasia; and 19% esophageal adenocarcinoma) were compared with 89 controls (no endoscopic evidence of BE; median age, 59 years; 47% male).
All participants swallowed the sponge, which was withdrawn after 8 minutes, and underwent subsequent EGD. DNA extracted from the sponge device was then subjected to methylation studies. Of the several methylated DNA markers tested, 5 (VAV3, ZNF682, NDRG4, FER1L4, and ZNF568) were selected using a cross-validated method for BE prediction. The sensitivity of these 5 markers was 92% (95% confidence interval [CI], 85%–96%) and the specificity was 94% (95% CI, 87%–98%), with an overall area under the curve of 0.97 (95% CI, 0.93-0.99). There was no significant difference in the sensitivity for BE without dysplasia (89%; 95% CI, 77%–96%) compared with BE with any grade of dysplasia (95%; 95% CI, 85%–99%) (P=.16). The prediction model was not affected by age, sex, body mass index, or smoking status, but it was influenced by BE length (4 cases of short-segment BE missed; P<.0001). Complications with the device included technical issues (5 patients), intolerance/premature withdrawal <5 minutes (4 patients), or tether detachment (1 patient).

COMMENTUsing a sponge on a string and combining it with biomarkers is a safe and promising option for BE diagnosis, but it needs to be evaluated in larger randomized controlled trials. EGD continues to be the gold standard for BE screening.
Note to readers: At the time we reviewed this paper, its publisher noted that it was not in final form and that subsequent changes might be made.
CITATION(S)
Iyer PG, Taylor WR, Johnson ML, et al. Accurate nonendoscopic detection of Barrett’s esophagus by methylated DNA markers: a multisite case control study. Am J Gastroenterol 2020 Jun 15. (Epub ahead of print) (https://doi.org/10.14309/ajg.0000000000000656)