Paris Classification Early Cancer
Alexander Meining (Ulm) and Thomas Rösch (Hamburg)
Endoscopic treatment for early carcinoma in the gastrointestinal tract has in the meantime become evidence-based and has been incorporated into national and international guidelines [1–3]. However, endoscopic therapy in the upper GI tract is only indicated for lesions that are limited to the mucosa, or at most the very superficial submucosa. In the lower GI tract, the definition of carcinoma first starts with submucosal infiltration, while “mucosal carcinomas” are equivalent to high-grade dysplasia in terms of their biological behavior; the term “mucosal cancer” should therefore not be used clinically.
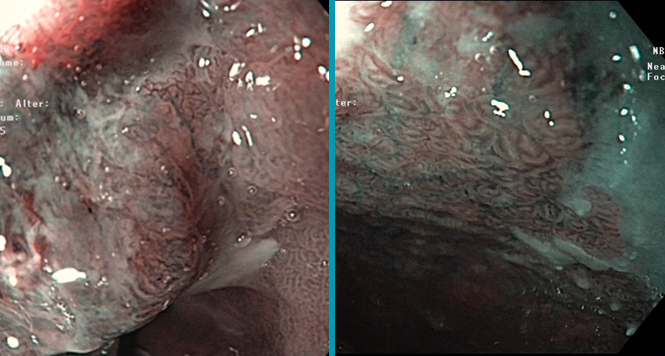
Generally, the endoscopic appearance here can already provide an initial, approximate assessment of the depth of infiltration (into the mucosa or beyond) and can guide the subsequent management. The Paris classification, based on earlier Japanese classifications, was developed to allow morphological classification of superficial lesions [4,5]. The Paris classification should therefore be regarded as a part of standard endoscopic terminology.
The Paris classification of early and/or superficial tumors in the GI tract was developed by an international consortium, in a two-stage process to date. Superficial or early neoplasias in the entire GI tract are primarily assessed on the basis of their endoscopic appearance and are defined as type 0 (for other types, see the endoscopic classification of advanced tumors); the “0” is usually omitted in clinical practice — for example, “type IIa” instead of “type 0-IIa.”
The figure from the relevant paper [5] provides diagrammatic representations of the different shapes of tumor:

Typ 0-I indicates elevated or polypoid forms, namely
0-Ip Polypoid/pedunculated
0-Is Polypoid/sessile, broad-based
Typ 0-II indicates flat or superficial forms, namely
0-IIa Flat and elevated
0-IIb Completely flat
0-IIc Superficially depressed
These types often consist of mixed forms — e.g., type IIa+c = flat and elevated with a central depression.
Typ 0-III indicates excavated forms, without any further subgrouping:
0-III Excavated/ulcerated
Types II and III are also referred to as nonpolypoid forms, as distinct from type I.
An overview of all the tumor types, including mixed forms, is shown below:

The boundaries between the definitions are sometimes not absolutely clear; this is reflected in the fact that the category “superficial” is a subgroup (0-II) in a classification of superficial lesions (as in the title). In principle, the classification [5] thus strictly speaking does not define “early lesions,” but rather “superficial lesions,” as those that should be regarded as either noninvasive (low-grade and high-grade dysplasia, or intraepithelial dysplasia) or as corresponding to stage T1 (m and sm) — i.e., early carcinomas. Later in the text, it is mentioned that this classification “includes” lesions that are basically amenable to curative endoscopic therapy. This in turn — again, strictly speaking — only represents a subgroup of early lesions (although a large one), namely mucosal cancers in the esophagus and stomach and submucosal cancers (with superficial infiltration) in the colorectum. In other words, a precise distinction between mucosal and submucosal invasive early carcinomas (i.e., the distinction between lesions that are endoscopically resectable and those that are not resectable) is not provided by the Paris classification. Other morphological classification systems (based on the superficial structure and pit patterns, etc.), mainly developed by colleagues in the Far East, are therefore used here.
The Paris classification attempts to achieve a precise morphological definition based on measurements, but in view of the lack of precision of endoscopic assessments, this is unrealistic. Elevated/polypoid lesions (0-I) are defined as having more than double the amount of mucosal thickness in a histological specimen, while flat lesions (0-II) are less than that [1]. In the illustrations presented in the paper, an open biopsy forceps (2.5 mm) is mentioned as a reference value, with the height of polypoid lesions being assessed as greater and that of nonpolypoid ones as less. However, the accuracy of such estimates and whether they are really used in everyday clinical routine work is more than doubtful.

In American studies of colorectal polyps, a flat adenoma is defined as having a maximum height of 1.3 mm [6]. This is based on a histological study that showed that, based on the original definition by Muto et al. [7] — which is also used in the present classification (flat = polyp height less than two times the mucosal thickness) — 92% of all flat lesions came to 1.3 mm or less [8].
What are known as “laterally spreading tumors” (LSTs) are also included in the Paris classification. These in turn have varying “malignant potential” (a separate presentation of the classification of these will be provided shortly).
The clinical implications of the classification mainly involve the assessment of endoscopic resectability. Lesions that clearly protrude into the lumen (type I) and those that grow predominantly at the level of the surrounding mucosa (type II) are usually amenable to endoscopic resection. In the ulcerated type (type III), there is a greater risk of deeper infiltration, which on the one hand technically hampers endoscopic resection, but on the other hand is also associated with a greater risk of lymph-node metastases. In these cases, a primary classical surgical procedure therefore needs to be considered. For type II lesions, combined findings have also been described, and type IIc is usually associated with more aggressive growth.
With regard to the topographic distribution, type I (and II) lesions are frequent in the colorectum, while type II tumors are predominantly found in the esophagus and stomach. Type III lesions are relatively rare and are found more frequently in the upper GI tract (particularly the esophagus) [4].
References
- Japanese Gastric Cancer Association. Japanese gastric cancer treatment guidelines 2014 (ver. 4). Gastric Cancer. 2017 Jan;20(1):1-19.
- Pimentel-Nunes P, Dinis-Ribeiro M, Ponchon T, et al.. Endoscopic submucosal dissection: European Society of Gastrointestinal Endoscopy (ESGE) Guideline. Endoscopy. 2015 Sep;47(9):829-54.
- Moehler M, Al-Batran SE, Andus T, et al. [German S3-guideline “Diagnosis and treatment of esophagogastric cancer”]. Z Gastroenterol. 2011 Apr;49(4):461-531.
- The Paris endoscopic classification of superficial neoplastic lesions: esophagus, stomach, and colon: November 30 to December 1, 2002.[No authors listed]. Gastrointest Endosc. 2003 Dec;58(6 Suppl):S3-43.
- Endoscopic Classification Review Group. Update on the paris classification of superficial neoplastic lesions in the digestive tract. Endoscopy. 2005;Jun;37(6):570-8.
- O’Brien MJ, Winawer SJ, Zauber AG, Bushey MT, Sternberg SS, Gottlieb LS, Bond JH, Waye JD, Schapiro M; National Polyp Study Workgroup. Flat adenomas in the National Polyp Study: is there increased risk for high-grade tdysplasia initially or during surveillance? Clin Gastroenterol Hepatol 2004;2:905–911.
- Muto T, Kamiya J, Sawada T, Konishi F, Sugihara K, Kubota Y, Adachi M, Agawa S, Saito Y, Morioka Y. Small flat adenoma of the large bowel with special reference to its clinicopathologic features. Dis Colon Rectum 1985;28:847–851.
- Cairns A, Dixon MF, Rembacken B, Finan PJ, Axon ATR, Quirke P. Flat adenomas—a distinct biological entity and a new definition. Gut 1999;44:TH566.