Image Challenges
Image Challenge
Question:
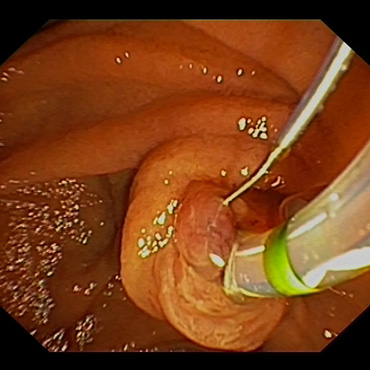
ERCP — bile duct perforation
What happened?
A patient with classic choledocholithiasis and colic pains undergoes ERCP for stone removal. The patient is in a relatively good general condition, but is receiving immunosuppression due to concomitant conditions.
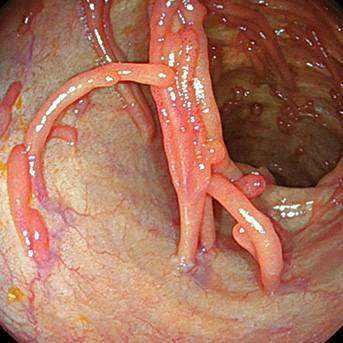
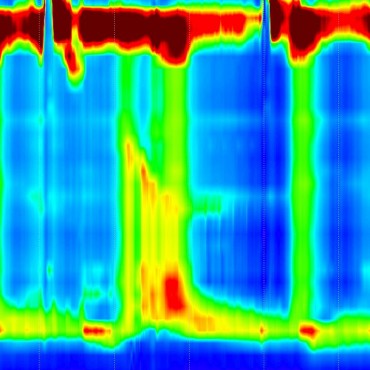
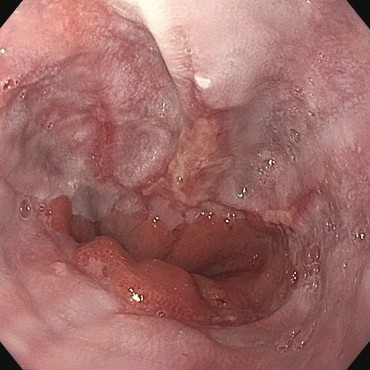
As intubation of the papilla is unsuccessful, a needle-knife precut procedure is carried out. Intubation is still not possible. ERCP is carried out on the following day by an experienced colleague. The needle-knife precut is enlarged. Intubation is still not possible. The patient’s general condition deteriorates, with increasing abdominal symptoms. Tomographic imaging raises a suspicion of bile duct perforation.
Subsequent PTCD is successful, with conversion to normal biliary stenting. The patient’s condition continues to deteriorate, with abscess formation in the retroperitoneal space. Placement of several suction drains. Due to the prior disease and pleural effusions, the patient has to be intubated. Difficult course continues, with retroperitoneal abscess formation. Surgical treatment with placement of a large-lumen catheter is carried out. Improvement is only gradual, partly due to the respiratory situation.
Suggestions for improvement by the notifying physician
The repeat ERC after the needle-knife precut may have been too early. The first colleague treating the patient did not have an experienced colleague behind him to call on. The immunosuppression was underestimated. Broad-spectrum antibiotic treatment would already have been desirable in the initial stage.
Feed back of our CIRS team:
Feedback from the CIRS team
It would probably have been better to end the first intervention even before attempting the needle-knife papillotomy, since at that time point a physician with experience in the technique was not available as a back-up. Needle-knife papillotomy following an unsuccessful precut papilla is difficult even for experienced physicians.
A pause of 2 days between the interventions could possibly have improved the prospects for the repeat intervention, as a result of further decongestion.
Primary antibiotic prophylaxis in patients with immunosuppression without neutropenia is not recommended in the “Quality Requirements in Gastrointestinal Endoscopy” guideline. Successful needle-knife papillotomy is also not an indication for prophylactic administration. With repeated interventions in ERCP, as in this case, antibiotic prophylaxis makes sense as an individual decision, in view of the immunosuppression.
When there is suspected perforation in ERCP, CT should be carried out immediately. If it is confirmed, antibiotic treatment must be started.
Ref.: Denzer U et al. S2k-Leitlinie Qualitätsanforderungen in der gastrointestinalen Endoskopie. Z Gastroenterol 2015; 53: E1–E227