Image Challenges
Image Challenge
Question:
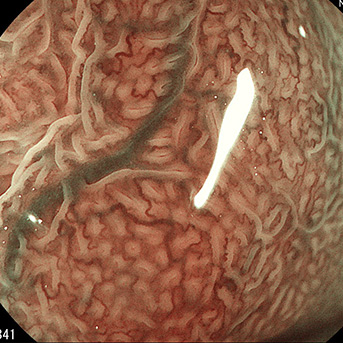
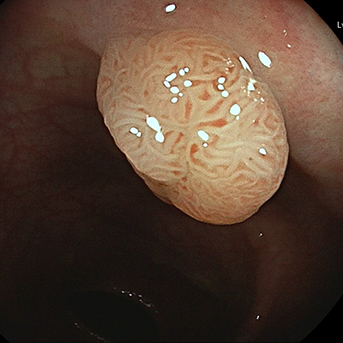
Elective admission for in-patient treatment of achalasia using peroral endoscopic myotomy (POEM).
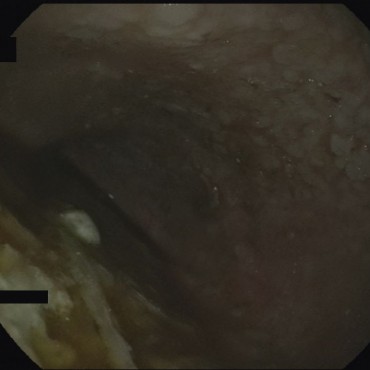
POEM was performed with the patient under intubation anesthesia, using a standard gastroscope and low-flow CO2 insufflation.
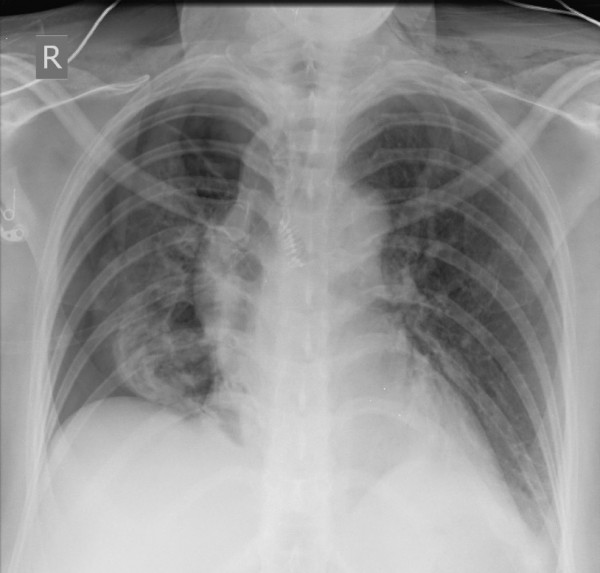
During the course of the procedure, insufflation of room air was accidentally activated after the endoscopy processor had been re-started. Marked cutaneous emphysema and pneumothorax developed.
Feed back of our CIRS team:
Suggestions for improvement by the person reporting:
After re-setting of the endoscopy processor during any procedure that may interrupt or endanger the continuity of the intestinal wall — especially tunnel techniques — an active check should be made that insufflation of room air has been switched off, to ensure that CO2 alone (preferably with low flow) is insufflated.
In the end, the good level of experience in the team on both the endoscopy and anesthesia sides led to a good outcome for the patient. Especially at the start of the learning curve for this type of intervention in both specialties, particular attention needs to be given to these details, since technical aspects are often initially the greatest challenge. Although the complication rate with CO2 insufflation is low, this type of intervention should only be carried out if the appropriate level of experience and the infrastructure needed to manage complications are available.
Feedback from the CIRS team:
POEM has in the meantime become an established treatment option for achalasia. It is safe in principle, but requires expertise during the procedure and in the management of complications.
The iatrogenically created connection between the esophageal lumen and the mediastinum, pleura, or peritoneum means that the insufflated CO2 can flow into the respective compartments and thus lead to systemic CO2 accumulation, capnomediastinum, tension capnoperitoneum, or pneumothorax [1].
Performing POEM (or other transmural interventions) with room air is now obsolete. A study by Cai et al., for example, showed that using CO2 markedly reduces the incidence of mediastinal and cutaneous emphysema and pneumoperitoneum. The incidence of pneumothorax requiring treatment was also significantly reduced [2]. Cases have been reported of accidental air embolisms, including cerebral air embolisms, during extraluminal air insufflation (e.g., also if perforation occurs during ERCP), with neurological damage and deaths.
After a light source/processor has been re-started during endoscopy, the air supply does not switch on automatically. To prevent the wrong button from being pressed in a reflex response (introducing room air instead of CO2), the room air button could be taped over before the intervention starts. Particularly in endoscopy units that work with CO2 less often, it is advisable to provide staff with regular training on the purpose of using CO2.
References
- Löser B, Werner YB, Löser A, Rösch T, Petzoldt M. Anästhesie in der gastrointestinalen Endoskopie: perorale endoskopische Myotomie. Anaesthesist 2019; 68: 607–614.
- Cai M-Y, Zhou P-H, Yao L-Q, Zhu B-Q, Liang L, Li Q-L. Thoracic CT after peroral endoscopic myotomy for the treatment of achalasia. Gastrointest Endosc 2014; 80: 1046–1055.