Image Challenges
Image Challenge
Question:
The patient was admitted with progressive diarrhea and increasing nausea and vomiting, dehydrated, and in poor general condition, with normal weight.
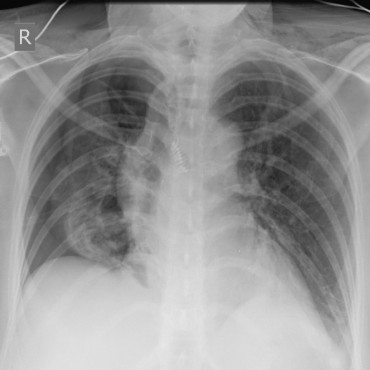
Metastatic pancreatic carcinoma. Status post partial pancreatic resection with ablation of the left colic flexure, duodenojejunal flexure, resection of the posterior wall of the stomach, segmental hepatic resection, and splenectomy. Status post adjuvant chemotherapy. Pulmonary metastases developed during the course.
Computed tomography:
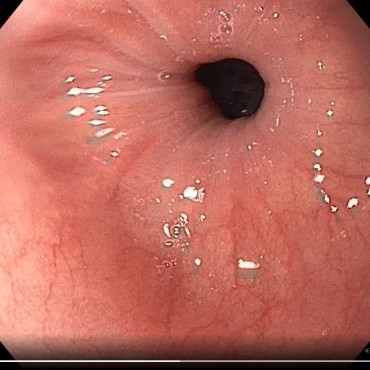
1. At the level of the duodenojejunostomy, there was clear, subtotally stenotic wall thickening with subsequent prestenotic dilation of the duodenum. Differential diagnosis: caused by tumor.
2. Status post partial hepatic resection, currently with no evidence of hepatic metastases. No pathologically enlarged intra-abdominal lymph nodes, but some suspicion of peritoneal carcinosis in the mid-abdomen ventrally.
3. Pleural effusion and large pulmonary metastases in the left lower area of the lung. This gave rise to the indication for endoscopic stent treatment.
Feed back of our CIRS team:
Treatment:
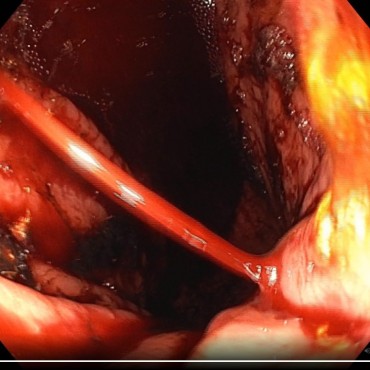
The stenosis caused by tumor infiltration, approximately 6 cm distal to the papilla, was bridged under fluoroscopic guidance by placing a self-expanding uncovered metal stent, 11 cm long. An existing fistula formation from the duodenum to the colon was stented in the process. This created a short-bowel situation, with progressive diarrhea. This was not initially recognized.
On the following day, during clarification of a bowel wall thickening that had been reported on imaging, a sigmoidoscopy was carried out. The incorrect positioning of the stent was recognized, confirmed on CT, and then successfully corrected surgically – with en bloc resection with the transverse colon, small bowel, blind closure of the duodenum behind the ligament of Treitz, re-anastomization of the jejunum to the proximal duodenum, jejunojejunostomy and transverso-transversostomy.
Reasons for the unfavorable course:
The fistula formation between the duodenum, with its tumor-related stenosis, and the colon was already visible on the preinterventional CT, but it was not reported as such and was not recognized by the endoscopist.
Suggestions for improvement by the person reporting:
Better demonstration and communication of the radiological findings. Examination of the imaging findings by the endoscopist before the intervention. Early interdisciplinary discussion of the case might have avoided this situation.
Feedback from the CIRS team:
This case involves a quite rare situation, but one with tremendous consequences for the patient. There is no question that it is indispensable for the endoscopist to look at the CT imaging before an examination. When there are complex findings, experience shows that the radiological report alone is not sufficient. The radiologist often lacks important information when reporting on the radiographic images. As is true throughout the world – not only in medicine – the following quotation is universally applicable: “You only see what you already know and understand” [1]. As the person reporting has already stated in the analysis, an interdisciplinary discussion can be recommended when there are complex findings.
Reference
- Goethe JW von. [Conversation noted by Friedrich von Müller, April 24, 1819]. In: Beutler E, editor. Gedenkausgabe der Werke, Briefe und Gespräche. Vol. 23, Pfeiffer-Belli W, editor. Goethes Gespräche. Zweiter Teil. Zurich: Artemis-Verlag; 1950. p. 52.