Image Challenges
Image Challenge
Question:
What happened?
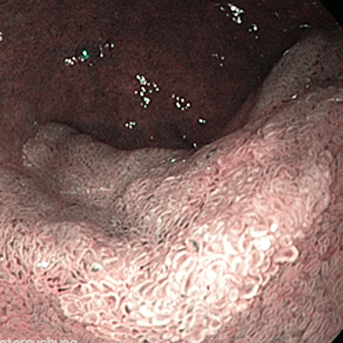
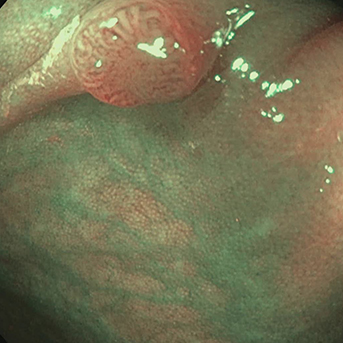
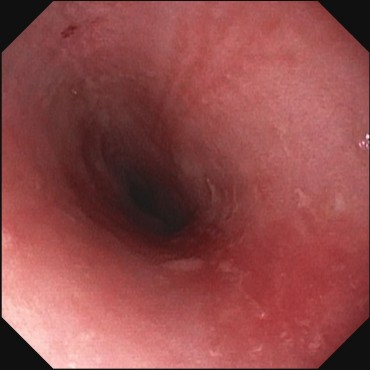
A patient known to have type I achalasia was to receive treatment with balloon dilation. After propofol administration (ca. 140 mg), sudden massive vomiting (certainly at least 500 mL) and consequent severe coughing. Protective reflexes were thus still well preserved. There was no drop in peripheral O2 saturation. The patient then received suction, and the examination was stopped.
Suggestions for improvement by the notifying physician:
It is possible that the patient was not asked how long he had fasted.
Feed back of our CIRS team:
In achalasia, the most frequent symptoms are dysphagia for solids and liquids, which is associated with food and liquid stasis in the esophagus [1]. The patients are also often reported to suffer aspiration. Particular caution is therefore needed when the patient is known to have achalasia. A current literature search did not identify any exact data on the frequency of aspiration or vomiting during endoscopy. However, experience shows that a liquid-filled esophagus is a frequent finding in achalasia and requires certain precautions to be taken. For example, the examination table should be tilted so that the head is elevated. An additional facility for suction should be available in all cases. Only a fluid diet should be taken for 1–2 days beforehand, and the last fluid intake should be at least 12 h before the examination. These recommendations are based on the CIRS team’s experience.
1. Fisichella PM, Raz D, Palazzo F, Niponmick I, Patti MG. Clinical, radiological, and manometric profile in 145 patients with untreated achalasia. World J Surg 2008; 32: 1974–1979.