Can We Improve Quality in ERCP and EUS?
Vanessa M. Shami, MD, FASGE, reviewing Keswani RN, et al. Gastrointest Endosc 2023 Mar 24.
ERCP and EUS are essential in treating a variety of disease entities. Metrics exist to measure performance quality, but data are necessary to improve quality when deficiencies are identified. Authors of a new practice guideline from the American Society for Gastrointestinal Endoscopy systematically examined the published 2016 priority indicators for ERCP and EUS and reviewed the literature to identify interventions to enhance the quality of the priority indicators. These interventions could be used by providers and endoscopy centers falling below reported benchmarks for these indicators.
Quality indicators and interventions that might improve ERCP quality
Appropriate indication and documentation of the indication in >90% of cases:
- Audit and feedback
Cannulation rate in patients without surgically altered anatomy in >90% of cases:
- Prone position versus other positions
- Deep versus moderate sedation
- Sphincterotomes versus cannulas
- Physician-controlled wire-guided cannulation versus standard techniques
- Limited data on educational interventions using mechanical simulators for trainees and advanced cannulation techniques to improve cannulation success rates with high-volume endoscopists
The extraction rate of stones <1 cm in >90% of cases:
- Extraction balloon versus basket in select cases
- Sphincteroplasty with or without sphincterotomy versus sphincterotomy alone
- Cholangioscopy or intraductal ultrasound in select cases
Stent placement rate for biliary obstruction below the bifurcation in patients with nonsurgically altered anatomy in >90% of cases:
- Guidewires with a stiff shaft and hydrophilic tip versus standard wires
- Dilators (graduated catheters, stent retrievers, hydrostatic balloons)
Post-ERCP pancreatitis (rate not available/identified):
- Physician-controlled wire-guided cannulation
- Rectal indomethacin in high-risk patients
- Aggressive periprocedural hydration with lactated Ringer’s solution
- Pancreatic stents in patients with inadvertent pancreatic duct cannulation
Quality indicators and interventions that might improve EUS quality
The frequency with which all GI cancers are staged with the American Joint Committee on Cancer/International Union Against Cancer tumor, node, metastasis staging system (should be >98%):
- Audit and feedback
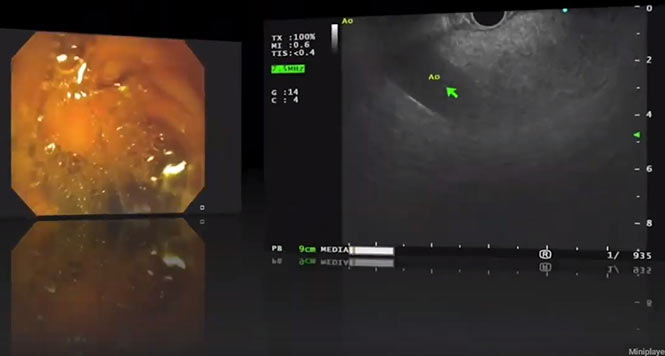
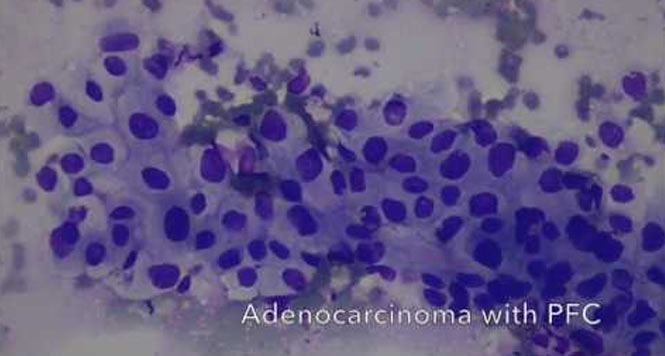
Diagnostic rates and sensitivity for malignancy in solid pancreatic masses (>70% in patients with a pancreatic mass with a sensitivity for malignancy of >85% among all pancreatic cancers):
- Negative pressure suction or slow-pull and fanning technique
- Limited data for deep versus moderate sedation and core biopsy versus fine-needle aspiration (FNA), especially when rapid onsite cytopathology evaluation is unavailable
Reducing adverse events after EUS-FNA (acute pancreatitis <2%, perforation <0.5%, bleeding <1%, infection N/A):
- Selective antibiotic use
- Discontinue antithrombotic therapy when FNA/fine-needle biopsy is anticipated

COMMENTWhile quality metrics have been proposed for several years — most with thresholds defining low versus high performers — this paper identifies that few robust interventions improve ERCP and EUS quality. Moreover, most institutions are not tracking many of these quality metrics for their ERCP and EUS practitioners. In sum, this paper highlights that more work and data are needed to make quality metrics tracking more feasible, to identify interventions to improve the quality of these procedures, and to implement them more routinely in practice.
Note to readers: At the time we reviewed this paper, its publisher noted that it was not in final form and that subsequent changes might be made.
CITATION(S)
Keswani RN, Duloy A, Nieto JM, et al. Interventions to improve the performance of ERCP and EUS quality indicators. Gastrointest Endosc 2023 Mar 24. (Epub ahead of print) (https://doi.org/10.1016/j.gie.2022.12.010)