Low Incidence of Colorectal Cancer After Endoscopic Dysplasia Resection in Patients With IBD
Monika Fischer, MD, reviewing Mohan BP, et al. Gastrointest Endosc 2020 Jun 24.
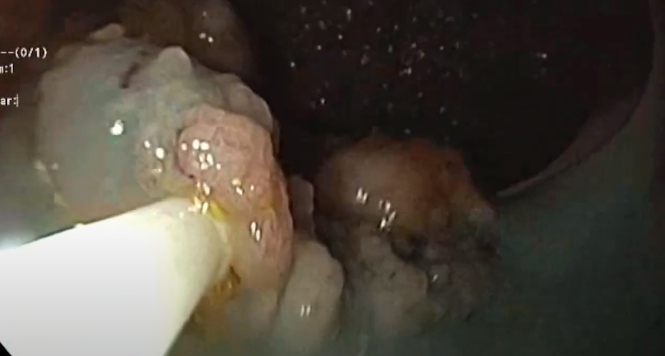
Given the paucity of high-quality outcome data, the optimal management of polypoid and/or nonpolypoid colonic lesions in IBD is an ongoing debate. Guidelines recommend that dysplasia with distinct margins be considered for endoscopic resection, followed by close colonoscopic surveillance.
The authors conducted a meta-analysis of 18 studies involving 1037 patients (933 with ulcerative colitis) with a total of 1428 lesions endoscopically resected from the colon who were followed for a mean duration ranging from 6 months to 82 months. The pooled risk of colorectal cancer (CRC) and high-grade dysplasia (HGD) was estimated to be 2 per 1000 person-years of follow-up. The incidence and/or recurrence rate of any lesion was 43 per 1000 person-years, with one-third of lesions managed endoscopically. Lesion location (right, left), size, type (Paris-I, Paris-II), or histology (low-grade dysplasia [LGD], HGD) and endoscopic resection technique (EMR, ESD, or traditional polypectomy) did not influence the pooled outcomes of any neoplasia. While lesion characteristics did not significantly impact CRC risk, there were trends toward significance with left-sided lesions (P=.06) and lesion size (P=.06), supporting the notion that left-sided lesions, as well as large lesions, are more prone to malignant conversion. There were also trends toward significance with both LGD (P=.06) and HGD (P=.09), supporting the hypothesis that tumor progression in an inflammatory bowel segment does not necessarily follow the LGD to HGD to cancer pathway. The rate of adverse events was low at 2% for each bleeding and perforating complication.

COMMENTThis meta-analysis supports endoscopic management of clearly visible, endoscopically removable dysplastic lesions in IBD. Due to a small sample size, however, this study was unable to compare outcomes between different resection techniques, such as cold or hot snare polypectomy, EMR, and ESD.
Note to readers: At the time we reviewed this paper, its publisher noted that it was not in final form and that subsequent changes might be made.
CITATION(S)
Mohan BP, Khan SR, Chandan S, et al. Endoscopic resection of colon dysplasia in patients with inflammatory bowel disease: a systematic review and meta-analysis. Gastrointest Endosc 2020 Jun 24. (Epub ahead of print) (https://doi.org/10.1016/j.gie.2020.06.048)