Fecal DNA testing — a new threat to screening colonoscopy?
Thomas Rösch, Hamburg and Michael Bretthauer, Oslo
The New England Journal of Medicine
| Multitarget Stool DNA Testing for Colorectal-Cancer Screening |
| Thomas F. Imperiale, M.D., David F. Ransohoff, M.D., Steven H. Itzkowitz, M.D., Theodore R. Levin, M.D., Philip Lavin, Ph.D., Graham P. Lidgard, Ph.D., David A. Ahlquist, M.D., and Barry M. Berger, M.D. |
Background
An accurate, noninvasive test could improve the effectiveness of colorectal-cancer screening.
Methods
We compared a noninvasive, multitarget stool DNA test with a fecal immunochemical test (FIT) in persons at average risk for colorectal cancer. The DNA test includes quantitative molecular assays for KRAS mutations, aberrant NDRG4 and BMP3 methylation, and β-actin, plus a hemoglobin immunoassay. Results were generated with the use of a logistic-regression algorithm, with values of 183 or more considered to be positive. FIT values of more than 100 ng of hemoglobin per milliliter of buffer were considered to be positive. Tests were processed independently of colonoscopic findings.
Results
Of the 9989 participants who could be evaluated, 65 (0.7%) had colorectal cancer and 757 (7.6%) had advanced precancerous lesions (advanced adenomas or sessile serrated polyps measuring ≥1 cm in the greatest dimension) on colonoscopy. The sensitivity for detecting colorectal cancer was 92.3% with DNA testing and 73.8% with FIT (P = 0.002). The sensitivity for detecting advanced precancerous lesions was 42.4% with DNA testing and 23.8% with FIT (P<0.001). The rate of detection of polyps with high-grade dysplasia was 69.2% with DNA testing and 46.2% with FIT (P = 0.004); the rates of detection of serrated sessile polyps measuring 1 cm or more were 42.4% and 5.1%, respectively (P<0.001). Specificities with DNA testing and FIT were 86.6% and 94.9%, respectively, among participants with nonadvanced or negative findings (P<0.001) and 89.8% and 96.4%, respectively, among those with negative results on colonoscopy (P<0.001). The numbers of persons who would need to be screened to detect one cancer were 154 with colonoscopy, 166 with DNA testing, and 208 with FIT.
Conclusions
In asymptomatic persons at average risk for colorectal cancer, multitarget stool DNA testing detected significantly more cancers than did FIT but had more false positive results. (Funded by Exact Sciences; ClinicalTrials.gov number, NCT01397747.)
What you need to know
Fecal tests have increasingly moved on from the classic fecal occult blood test (FOBT) to fecal immunologic testing (FIT), particularly in countries with newly introduced screening programs such as the Netherlands (1–5). The search is of course not only for carcinomas (in the early stage if possible), but also for colorectal adenomas. Advanced adenomas (< 1 cm, with villous components, high-grade dysplasias) are the most important and are also used as assessment parameters in many studies. In one study conducted before it was introduced, the level of acceptance for FIT was surprisingly higher than that for FOBT (61.5% vs. 49.5%), on the one hand. On the other, the yield for advanced adenomas was also higher (2.4% vs. 1.1%) (5). However, the performance of various FIT tests is highly varied (6–8). In the Netherlands, what is known as the OC Sensor Test is used (Eiken Chemical, Tokyo); in the study examined here, the OC FIT-CHEK test was used (Polymedco, Cortland Manor, New York). In Germany, the OC Sensor Test was compared with two other FIT tests, without any substantial differences being found between them (sensitivity for advanced adenomas 20–25%, specificity 95–97%) (10).
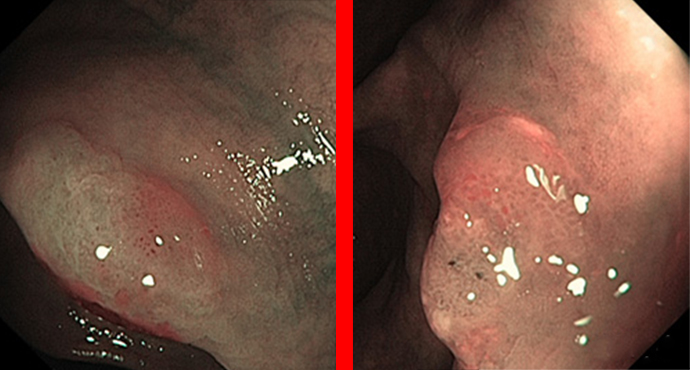
A fecal DNA test that was presented several years ago (12, 13) has now been tested in a large American study (14) in comparison with FIT, with colonoscopy as the gold standard. Overall, more than 12,000 individuals were included in the study, with 9989 ultimately included in the analysis; 65 had carcinomas on colonoscopy, 757 had advanced adenomas, and 2893 had adenomas that were not advanced and therefore usually small. In 6274 participants, nothing was found. The patients had to provide fecal samples before colonoscopy preparation (without dietary limitations). The gold standard was screening colonoscopy in each case, which in 90% of cases had been carried out within nearly the previous 18 months.
The results (14) show, with a limited number of carcinomas (n = 65), a sensitivity of 92%, and for advanced adenomas 42%; these values were approximately 20% superior to those with the FIT test. The specificity was 87%, and thus slightly poorer than FIT (95%). The detailed figures were as follows:
| Sensitivity for | n | Fecal DNA | FIT |
|---|---|---|---|
| Carcinoma | 65 | 92.3% | 73.8% |
| Stage I–III carcinomas | 60 | 93.3% | 73.3% |
| Carcinoma and HGD | 104 | 83.7% | 63.5% |
| Advanced adenomas | 757 | 42.4% | 23.8% |
| Non-advanced adenomas | 2893 | 17.2% | 7.6% |
| Specificity for | |||
| Normal colonoscopy | 4457 | 89.8% | 96.4% |
| Normal colonoscopy + non-adv. adenomas | 9167 | 86.6% | 94.9% |
Limitations of the study include a certain element of patient selection and the unclear practicability of the test and acceptance for it. Uptake studies are certainly needed. Overall, out of an initial 12,766 individuals who provided informed consent, 1760 were excluded because consent was withdrawn or no colonoscopy was actually carried out. A total of 689 were excluded due to technical problems in collecting or analyzing the fecal samples (6.2%); the extent to which this would reflect possible everyday conditions later is unclear. A further 304 patients were excluded due to incomplete colonoscopy or colonoscopy without good preparation (2.8%), and in 34 cases the FIT test did not function. Overall, therefore, there was positive selection in relation to the research aims. Samples for fecal DNA assessment have to be supplied in a relatively large box (about the size of a shoe box), so that screening programs that require postage methods are currently still a challenge. Further studies, particularly in relation to acceptance and uptake, are needed in order to show whether this test could be incorporated into colon screening in everyday conditions. It certainly does not replace colonoscopy, but a good and practicable filter test will eventually reduce colonoscopies to mainly therapeutic procedures, while at the same time potentially increasing the numbers due to greater acceptance of this type of screening test. Blood tests are currently not yet a reality for widespread application (15).
References
- de Wijkerslooth TR, Stoop EM, Bossuyt PM, Meijer GA, van Ballegooijen M, van Roon AH, Stegeman I, Kraaijenhagen RA, Fockens P, van Leerdam ME, Dekker E, Kuipers EJ. Immunochemical fecal occult blood testing is equally sensitive for proximal and distal advanced neoplasia. Am J Gastroenterol. 2012 Oct;107(10):1570-8. doi: 10.1038/ajg.2012.249. Epub 2012 Jul 31.
- Goede SL, van Roon AH, Reijerink JC, van Vuuren AJ, Lansdorp-Vogelaar I, Habbema JD, Kuipers EJ, van Leerdam ME, van Ballegooijen M. Cost-effectiveness of one versus two sample faecal immunochemical testing for colorectal cancer screening. Gut. 2013 May;62(5):727-34. doi: 10.1136/gutjnl-2011-301917. Epub 2012 Apr 5.
- van Roon AH, Goede SL, van Ballegooijen M, van Vuuren AJ, Looman CW, Biermann K, Reijerink JC, Mannetje H’, van der Togt AC, Habbema JD, van Leerdam ME, Kuipers EJ. Random comparison of repeated faecal immunochemical testing at different intervals for population-based colorectal cancer screening. Gut. 2013 Mar;62(3):409-15. doi: 10.1136/gutjnl-2011-301583. Epub 2012 Mar 2.
- Wilschut JA, Hol L, Dekker E, Jansen JB, Van Leerdam ME, Lansdorp-Vogelaar I, Kuipers EJ, Habbema JD, Van Ballegooijen M. Cost-effectiveness analysis of a quantitative immunochemical test for colorectal cancer screening. Gastroenterology. 2011 Nov;141(5):1648-55.e1. doi: 10.1053/j.gastro.2011.07.020. Epub 2011 Jul 22.
- Hol L, van Leerdam ME, van Ballegooijen M, van Vuuren AJ, van Dekken H, Reijerink JC, van der Togt AC, Habbema JD, Kuipers EJ. Screening for colorectal cancer: randomised trial comparing guaiac-based and immunochemical faecal occult blood testing and flexible sigmoidoscopy. Gut. 2010 Jan;59(1):62-8. doi: 10.1136/gut.2009.177089. Epub.
- Raginel T, Puvinel J, Ferrand O, Bouvier V, Levillain R, Ruiz A, Lantieri O, Launoy G, Guittet L.´A population-based comparison of immunochemical fecal occult blood tests for colorectal cancer screening. Gastroenterology. 2013 May;144(5):918-25. doi: 10.1053/j.gastro.2013.01.042. Epub 2013 Feb 1.
- Hundt S, Haug U, Brenner H. Comparative evaluation of immunochemical fecal occult blood tests for colorectal adenoma detection. Ann Intern Med. 2009 Feb 3;150(3):162-9.
- Hundt S, Haug U, Brenner H. Comparative evaluation of immunochemical fecal occult blood tests for colorectal adenoma detection. Ann Intern Med. 2009 Feb 3;150(3):162-9.
- Haug U, Hundt S, Brenner H. Quantitative immunochemical fecal occult blood testing for colorectal adenoma detection: evaluation in the target population of screening and comparison with qualitative tests. Am J Gastroenterol. 2010 Mar;105(3):682-90. doi: 10.1038/ajg.2009.668. Epub 2009 Dec 1.
- Brenner H, Tao S. Superior diagnostic performance of faecal immunochemical tests for haemoglobin in a head-to-head comparison with guaiac based faecal occult blood test among 2235 participants of screening colonoscopy. Eur J Cancer. 2013 Sep;49(14):3049-54. doi: 10.1016/j.ejca.2013.04.023. Epub 2013 May 22.
- von Karsa L, Patnick J, Segnan N. European guidelines for quality assurance in colorectal cancer screening and diagnosis. First Edition–Executive summary. Endoscopy. 2012 Sep;44 Suppl 3:SE1-8. Epub 2012 Sep 25.
- Ahlquist DA, Sargent DJ, Loprinzi CL, Levin TR, Rex DK, Ahnen DJ, Knigge K, Lance MP, Burgart LJ, Hamilton SR, Allison JE, Lawson MJ, Devens ME, Harrington JJ, Hillman SL. Stool DNA and occult blood testing for screen detection of colorectal neoplasia. Ann Intern Med. 2008 Oct 7;149(7):441-50, W81.
- Ahlquist DA, Zou H, Domanico M, Mahoney DW, Yab TC, Taylor WR, Butz ML, Thibodeau SN, Rabeneck L, Paszat LF, Kinzler KW, Vogelstein B, Bjerregaard NC, Laurberg S, Sørensen HT, Berger BM, Lidgard GP. Next-generation stool DNA test accurately detects colorectal cancer and large adenomas. Gastroenterology. 2012 Feb;142(2):248-56; quiz e25-6. doi: 10.1053/j.gastro.2011.10.031. Epub 2011 Nov 4.
- Imperiale TF, Ransohoff DF, Itzkowitz SH, Levin TR, Lavin P, Lidgard GP, Ahlquist DA, Berger BM: Multitarget Stool DNA Testing for Colorectal-Cancer Screening. NEJM online
- Church TR, Wandell M, Lofton-Day C, Mongin SJ, Burger M, Payne SR, Castaños-Vélez E, Blumenstein BA, Rösch T, Osborn N, Snover D, Day RW, Ransohoff DF; PRESEPT Clinical Study Steering Committee, Investigators and Study Team. Prospective evaluation of methylated SEPT9 in plasma for detection of asymptomatic colorectal cancer. Gut. 2014 Feb;63(2):317-25. doi: 10.1136/gutjnl-2012-304149. Epub 2013 Feb 13.